To Book an Appointment
HEARING EVALUATION
- Pure tone audiometry
- Immittance audiometry
- Speech audiometry
- Eustachian tube function test
- Special test
- Glycerol test
- Otoacoustic emission (OAE)
- New born hearing screening
- ABR/BERA (Auditory brainstem response)
- MLR (Middle latency response)
- LLR (Late latency response)
- P300
- MMN (Mis Match Negativity)
- VEMP (Vestibular evoked myogenic potential)
- Tinnitus Evaluation
- Electrocochleography (Ecocgh)
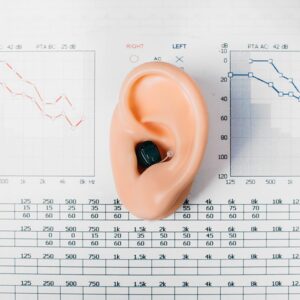
Pure tone audiometry or pure-tone audiometry is the main hearing test used to identify hearing threshold levels of an individual, enabling determination of the degree, type and configuration of a hearing loss and thus providing a basis for diagnosis and management.
Pure-tone audiometry is a subjective, behavioural measurement of a hearing threshold, as it relies on patient responses to pure tone stimuli. Therefore, pure-tone audiometry is only used on adults and children old enough to cooperate with the test procedure.
Pure-tone audiometry provides ear specific thresholds, and uses frequency specific pure tones to give place specific responses, so that the configuration of a hearing loss can be identified. As pure-tone audiometry uses both air and bone conduction audiometry, the type of loss can also be identified via the air-bone gap.

Immittance audiometry is an objective technique which evaluates middle ear function by three procedures: static immittance, tympanometry, and the measurement of acoustic reflex threshold sensitivity.
The primary purpose of impedance audiometry is to determine the status of the tympanic membrane and middle ear via tympanometry. The secondary purpose of this test is to evaluate acoustic reflex pathways, which include cranial nerves (CN) VII and VIII and the auditory brainstem.

The objective of speech audiometry testing is to measure patient’s ability to identify speech stimuli, to confirm results of pure tone audiometry and to rule out the presence of nonorganic hearing loss or retro-cochlear pathology.
The battery of speech audiometry tests includes speech detection threshold (SDT), speech recognition threshold (SRT) and word recognition score (WRS).
Word recognition test scores are often plotted on a graph. A point on this graph represents the percentage words correctly repeated by the patient at a specified intensity level from completed standardized list of words. Cochlear pathology tends to demonstrate a “plateau effect,” reaching a ceiling of performance at <100% and no improvement in the score despite a rise in intensity.


The assumption that an increase in endolymph volume, with its effect on labyrinthine membrane behavior producing in part, the hearing loss and vestibular deficit in Meniere’s disease has led to the administration of dehydrating agents like glycerol. The goal is to reduce the volume abnormalities in inner ear and produce a measurable change in response that is improvement in behavioral audiometric test scores.
Glycerol is administered orally to patients to reduce fluid abnormalities in the inner ear. It affects hearing temporarily (for a few hours), the results of which are measured by audiogram.
Most patients may suffer headache and nausea after drinking the glycerol for post-glycerol audiometric evaluation, which usually subsides after few hours.

Your ear is made up of three parts—the outer, the middle, and the inner ear. The OAE test is used to find out how well your inner ear, or cochlea, works. It measures otoacoustic emissions, or OAEs. These are sounds given off by the inner ear when responding to a sound. There are hair cells in the inner ear that respond to sound by vibrating. The vibration produces a very quiet sound that echoes back into the middle ear. This sound is the OAE that is measured.
If you have normal hearing, you will produce OAEs. If your hearing loss is greater than 25–30 decibels (dB), you will not produce these very soft sounds.
This test can also show if there is a blockage in your outer or middle ear. If there is a blockage, no sounds will be able to get through to the inner ear. This means that there will be no vibration or sounds that come back.
How the OAE is done?
A small earphone, or probe, is placed in your ear. The probe puts sounds into your ear and measures the sounds that come back. You do not need to do or say anything during the test. The person doing the test can see the results on the monitor screen.

The newborn hearing screening test helps identify babies who have permanent hearing loss as early as possible. This means parents can get the support and advice they need right from the start.
Hearing loss in babies
1 to 2 babies in every 1,000 are born with permanent hearing loss in 1 or both ears.
This increases to about 1 in every 100 babies who have spent more than 48 hours in intensive care.
Most of these babies are born into families with no history of permanent hearing loss.
Permanent hearing loss can significantly affect babies' development.
Finding out early can give these babies a better chance of developing language, speech, and communication skills.
It will also help them make the most of relationships with their family or carers from an early age.

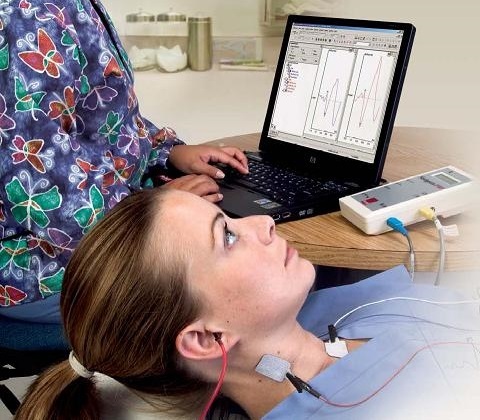
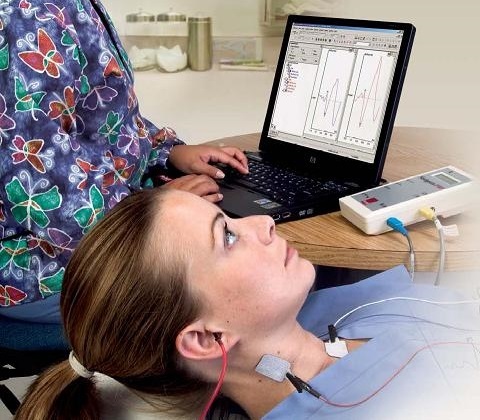
This is a test to evaluate the functioning of the inner ear and the hearing nerve. We can clarify hearing capabilities objectively without needing the patient’s active cooperation.
The test extracts electrical reactions along the hearing passage through to the brainstem.
The patient can be asleep or very relaxed during the test. If we are testing a baby, we can generally conduct the test without sedation or anesthetic up to the age of 5-6 months. Above that age and until a child can rest or sleep independently, the test is conducted under anesthetic.
The test is not invasive and does not hurt.
Electrodes are placed on the forehead and by the ears. An acoustic stimulation is transferred through a small earpiece lying at the entrance to the outer ear. In response to the stimulation transmitted at different volumes, the hearing nerve in the brainstem reacts accordingly.
We currently only perform this test for babies and children.

Auditory Middle-Latency Responses (AMLR) are related to auditory generators of the subcortical regions Na and Pa components at cortical levels. Na is considered the onset of the AMLR and Pa is considered the most robust component of the AMLR.
Why AMLR?
AMLR has the potential to offer a more complete picture of the status of the auditory system and can be used to help determine the degree of hearing loss. The most common neurological use of the AMLR is for the assessment of the functional integrity of the auditory pathway above the level of the brainstem in cases with suspected lesions and for the assessment of nonorganic hearing loss.
Further, AMLR is used in instances of traumatic brain injury, cortical deafness, multiple sclerosis, and cases of central auditory processing disorders.
Young children and infants may not present AMLR even when their auditory and neurological functions are intact, because of their higher sensitivity to stimulus rate. In general AMLR from children younger than 10 years should be interpreted with caution. It is also important to note that prior to the level of interest the auditory function should be examined and working normally, if not this will affect the AMLR results.
The stimuli used for AMLR is similar to the traditional ABR octave wide stimuli.
How to test
Patient Preparation is very important. The patient is instructed to relax and informed about the test procedure prior to testing. AMLR’s are most reliable when the patient is awake and quiet.
During sedation as with natural sleep the ALMR response is not affected.

Late Latency Response (LLR) is a component of auditory evoked potential response. The auditory evoked potential represents the cortical activity related to memory, attention, and auditory discrimination proficiency. The processing of acoustic signal occurs differently between verbal and non-verbal stimuli. These influence the amplitude and latency patterns.
The LLR response is found between 50 to 250 milliseconds from the time of stimulation. The test reflects the response of auditory cortex. LLR can acquire through pure tone stimulation by applying an envelope tone buster. The response is from a low frequency less than 30 Hz and has a frequent voltage of ranging between 3 to 10 microvolt’s.
The recordings have certain high points and low points. The peak depicts positive potential difference those are labelled as ‘P’ where as the low points depicts negative potential difference those are labelled as ‘N’. LLR responses are usually acquired by surface electrodes.
Why to take LLR test?
Late Latency Response test is used to diagnose certain conditions in auditory. This method of testing is very helpful in providing helpful information regarding hearing loss in patients with specific type of hearing disorder like with ‘c’ frequency. The LLR test can also help in testing the presence of nervous system abnormalities specifically above auditory brainstem levels.
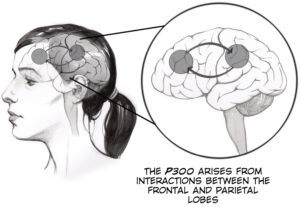
The P300 (P3) wave is an event-related potential (ERP) component elicited in the process of decision making. It is considered to be an endogenous potential, as its occurrence links not to the physical attributes of a stimulus, but to a person's reaction to it. More specifically, the P300 is thought to reflect processes involved in stimulus evaluation or categorization.
It is usually elicited using the oddball paradigm, in which low-probability target items are mixed with high-probability non-target (or "standard") items. When recorded by electroencephalography (EEG), it surfaces as a positive deflection in voltage with a latency (delay between stimulus and response) of roughly 250 to 500 ms.
The signal is typically measured most strongly by the electrodes covering the parietal lobe. The presence, magnitude, topography and timing of this signal are often used as metrics of cognitive function in decision-making processes. While the neural substrates of this ERP component still remain hazy, the reproducibility and ubiquity of this signal makes it a common choice for psychological tests in both the clinic and laboratory.

The mismatch negativity (MMN) or mismatch field (MMF) is a component of the event-related potential (ERP) to an odd stimulus in a sequence of stimuli. It arises from electrical activity in the brain and is studied within the field of cognitive neuroscience and psychology. It can occur in any sensory system, but has most frequently been studied for hearing and for vision. In the case of auditory stimuli, the MMN occurs after an infrequent change in a repetitive sequence of sounds (sometimes the entire sequence is called an oddball sequence.) For example, a rare deviant (d) sound can be interspersed among a series of frequent standard (s) sounds (e.g., s s s s s s s s s d s s s s s s d s s s d s s s s...). The deviant sound can differ from the standards in one or more perceptual features such as pitch, duration, or loudness. The MMN is usually evoked by either a change in frequency, intensity, duration or real or apparent spatial locus of origin.
The MMN can be elicited regardless of whether the subject is paying attention to the sequence. During auditory sequences, a person can be reading or watching a silent subtitled movie, yet still show a clear MMN. In the case of visual stimuli, the MMN occurs after an infrequent change in a repetitive sequence of images.
MMN refers to the mismatch response in electroencephalography (EEG); MMF or MMNM refer to the mismatch response in magnetoencephalography (MEG).
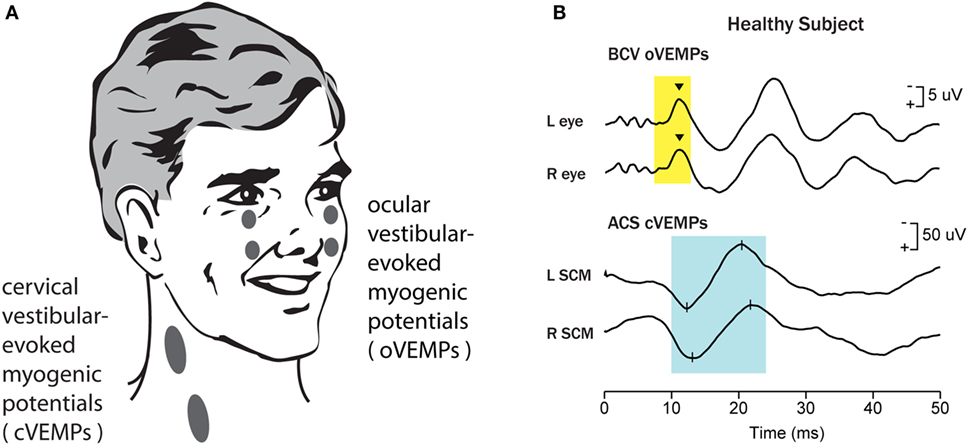
Vestibular evoked myogenic potential (VEMP) testing is a relatively new vestibular testing technique that determines vestibular function by applying a repetitive sound stimulus to one ear and then averaging the reaction of the muscle activity in response to each sound click or pulse.
Unlike caloric testing or rotational chair testing, VEMP does not measure eye movements. Surface EMG recordings over the ipsilateral sternocleidomastoid muscle (cervical VEMP [cVEMP]) is believed to assess function of the saccule. Surface EMG recordings over the contralateral inferior oblique (ocular VEMP [oVEMP]) is believed to assess function of the utricle.

The word tinnitus is derived from the Latin word tinnire, meaning “to ring” or “a ringing.” Tinnitus is defined as an unwanted auditory perception of internal origin, usually localized, and rarely heard by others.
Tinnitus takes different forms and has different classification proposals. One classification system stresses distinctions between vibratory and nonvibratory types, while another system groups the different forms of tinnitus into subjective or objective classes.
Vibratory tinnitus is caused by transmission to the cochlea of vibrations from adjacent tissues or organs. Nonvibratory tinnitus is produced by biochemical changes in the nerve mechanism of hearing.
Subjective tinnitus, which is more common, is heard only by the patient. Objective tinnitus can be heard through a stethoscope placed over head and neck structures near the patient's ear.
“Electrocochleography” (ECochG) is an investigation employed to measure electrical potentials of cochlea. The components of ECochG include measurement of cochlear potentials in response to a stimulus and measurement of the whole nerve or compound action potential (AP) of the eighth nerve.
Although the utility of ECochG diagnosis continues to be disputed, it has been proposed that in the situation that ECochG confirms the diagnosis of Meniere’s disease, one can be confident in deciding about an invasive therapy. What course be adopted when patient exhibits symptoms that confirm the diagnosis of Meniere’s disease, but ECochG is within normal limits remains a dilemma
Hearing Evaluation
Pure tone audiometry
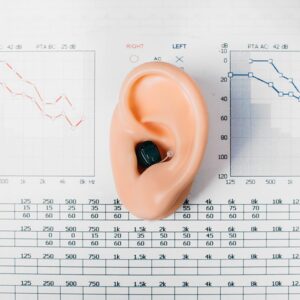
Pure tone audiometry or pure–tone audiometry is the main hearing test used to identify hearing threshold levels of an individual, enabling determination of the degree, type and configuration of a hearing loss and thus providing a basis for diagnosis and management.
Immittance audimetry

The primary purpose of impedance audiometry is to determine the status of the tympanic membrane and middle ear via tympanometry. The secondary purpose of this test is to evaluate acoustic reflex pathways, which include cranial nerves (CN) VII and VIII and the auditory brainstem.
Speech audiometry

The objective of speech audiometry testing is to measure patient’s ability to identify speech stimuli, to confirm results of pure tone audiometry and to rule out the presence of nonorganic hearing loss or retro-cochlear pathology.
Eustachian tube function test

Special test

Glycerol test

Glycerol is administered orally to patients to reduce fluid abnormalities in the inner ear. It affects hearing temporarily (for a few hours), the results of which are measured by audiogram.
Otoacoustic emission

The OAE test is used to find out how well your inner ear, or cochlea, works. It measures otoacoustic emissions, or OAEs. These are sounds given off by the inner ear when responding to a sound.
This test can also show if there is a blockage in your outer or middle ear. If there is a blockage, no sounds will be able to get through to the inner ear.
New born hearing screening

The newborn hearing screening test helps identify babies who have permanent hearing loss as early as possible. This means parents can get the support and advice they need right from the start.
ABR/BERA (Auditory brainstem response)

This is a test to evaluate the functioning of the inner ear and the hearing nerve. We can clarify hearing capabilities objectively without needing the patient’s active cooperation.
The test extracts electrical reactions along the hearing passage through to the brainstem. The patient can be asleep or very relaxed during the test. The test is not invasive and does not hurt.
MLR (Middle latency response)

Auditory Middle-Latency Responses (AMLR) are related to auditory generators of the subcortical regions Na and Pa components at cortical levels. Na is considered the onset of the AMLR and Pa is considered the most robust component of the AMLR.
LLR (Late latency response)

Late Latency Response (LLR) is a component of auditory evoked potential response. The auditory evoked potential represents the cortical activity related to memory, attention, and auditory discrimination proficiency. This method of testing is very helpful in providing helpful information regarding hearing loss in patients with specific type of hearing disorder like with ‘c’ frequency.
The LLR test can also help in testing the presence of nervous system abnormalities specifically above auditory brainstem levels.
P300
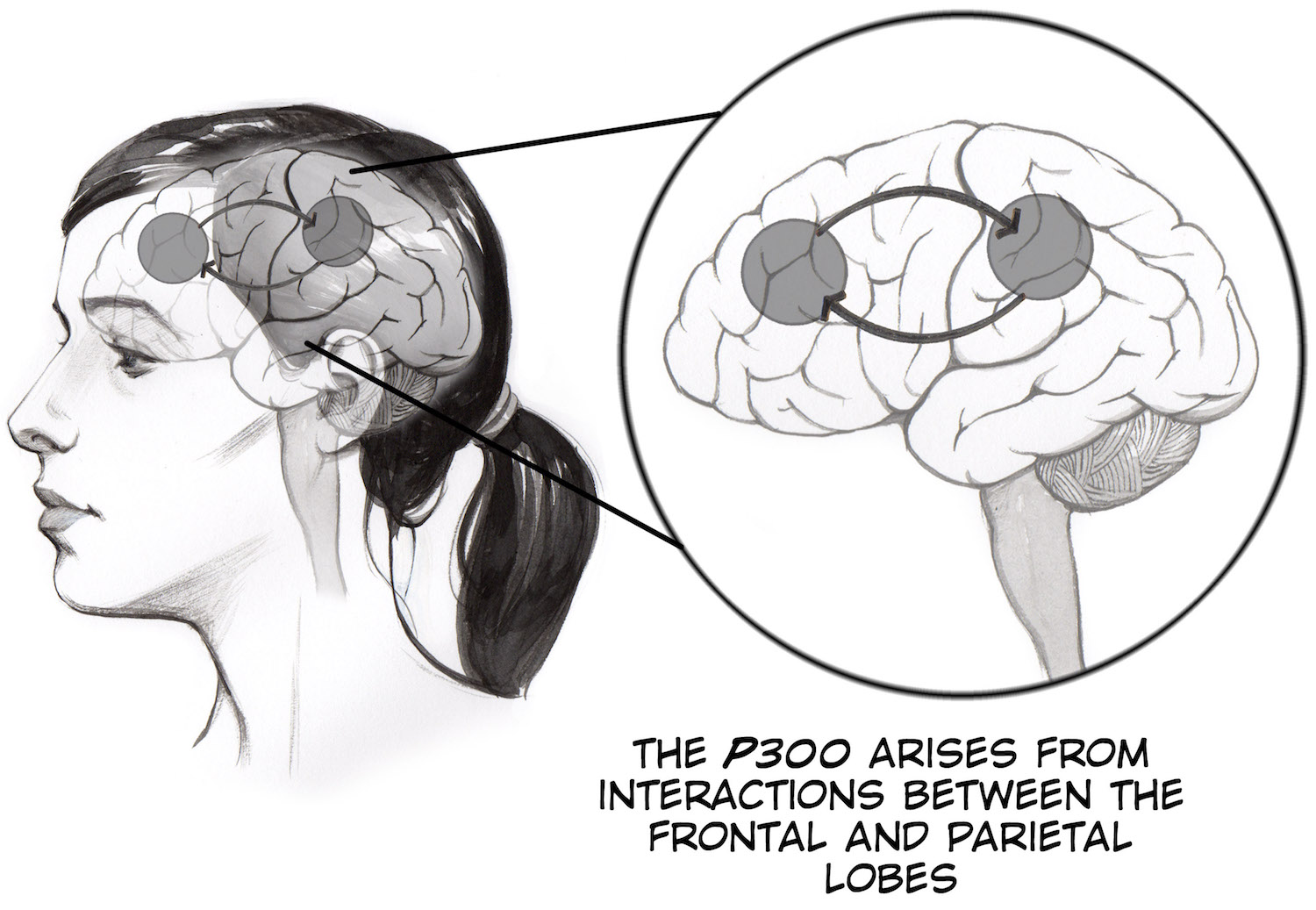
The P300 (P3) wave is an event-related potential (ERP) component elicited in the process of decision making. It is considered to be an endogenous potential, as its occurrence links not to the physical attributes of a stimulus, but to a person’s reaction to it. More specifically, the P300 is thought to reflect processes involved in stimulus evaluation or categorization.
MMN (Mis Match Negativity)

The mismatch negativity (MMN) or mismatch field (MMF) is a component of the event-related potential (ERP) to an odd stimulus in a sequence of stimuli. The MMN can be elicited regardless of whether the subject is paying attention to the sequence. During auditory sequences, a person can be reading or watching a silent subtitled movie, yet still show a clear MMN. In the case of visual stimuli, the MMN occurs after an infrequent change in a repetitive sequence of images.
VEMP (Vestibular evoked myogenic potential)
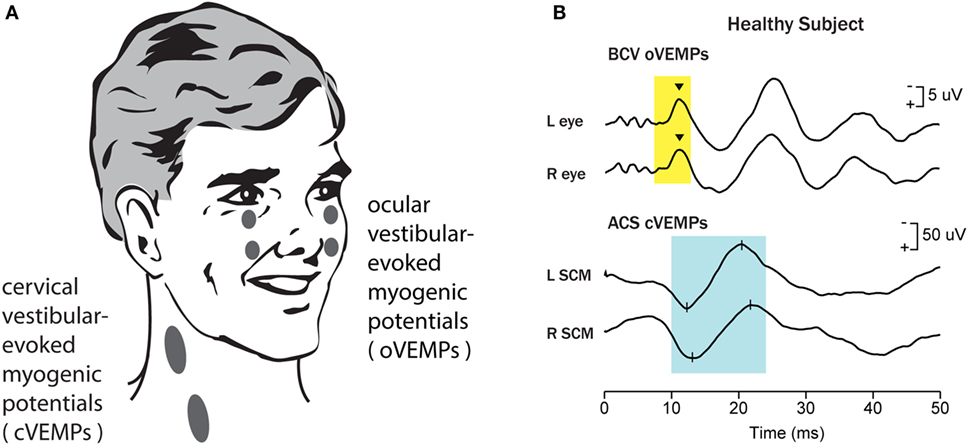
Vestibular evoked myogenic potential (VEMP) testing is a relatively new vestibular testing technique that determines vestibular function by applying a repetitive sound stimulus to one ear and then averaging the reaction of the muscle activity in response to each sound click or pulse. Unlike caloric testing or rotational chair testing, VEMP does not measure eye movements.
Tinnitus Evaluation

The word tinnitus is derived from the Latin word tinnire, meaning “to ring” or “a ringing.” Tinnitus is defined as an unwanted auditory perception of internal origin, usually localized, and rarely heard by others.
Electrocochleography (Ecocgh)
“Electrocochleography” (ECochG) is an investigation employed to measure electrical potentials of cochlea. The components of ECochG include measurement of cochlear potentials in response to a stimulus and measurement of the whole nerve or compound action potential (AP) of the eighth nerve.
